BRAIST STUDY
BRAIST STUDY
BRAIST STUDY
The role of bracing in patients with adolescent idiopathic scoliosis who are at risk for curve progression and eventual surgery is controversial.
Background
The role of bracing in patients with adolescent idiopathic scoliosis who are at risk for curve progression and eventual surgery is controversial.
Methods
We conducted a multicenter study that included patients with typical indications for bracing due to their age, skeletal immaturity, and degree of scoliosis. Both a randomized cohort and a preference cohort were enrolled. Of 242 patients included in the analysis, 116 were randomly assigned to bracing or observation, and 126 chose between bracing and observation. Patients in the bracing group were instructed to wear the brace at least 18 hours per day. The primary outcomes were curve progression to 50 degrees or more (treatment failure) and skeletal maturity without this degree of curve progression (treatment success).
Results
The trial was stopped early owing to the efficacy of bracing. In an analysis that included both the randomized and preference cohorts, the rate of treatment success was 72% after bracing, as compared with 48% after observation (propensity-score–adjusted odds ratio for treatment success, 1.93; 95% confidence interval [CI], 1.08 to 3.46). In the intention-to-treat analysis, the rate of treatment success was 75% among patients randomly assigned to bracing, as compared with 42% among those randomly assigned to observation (odds ratio, 4.11; 95% CI, 1.85 to 9.16). There was a significant positive association between hours of brace wear and rate of treatment success (P<0.001).
Conclusions
Bracing significantly decreased the progression of high-risk curves to the threshold for surgery in patients with adolescent idiopathic scoliosis. The benefit increased with longer hours of brace wear. (Funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and others; BRAIST ClinicalTrials.gov number, NCT00448448.)
Media in This Article Figure 1
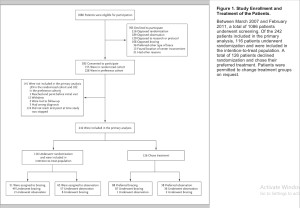
Study Enrollment and Treatment of the Patients.
Media in This Article Figure 2
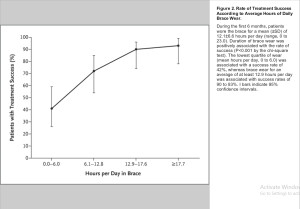
Rate of Treatment Success According to Average Hours of Daily Brace Wear.
Adolescent idiopathic scoliosis is characterized by a lateral curvature of the spine with a Cobb angle of more than 10 degrees and vertebral rotation. Whereas scoliosis develops in approximately 3% of children younger than 16 years of age, only 0.3 to 0.5% have progressive curves requiring treatment.1 Curves larger than 50 degrees are associated with a high risk of continued worsening throughout adulthood and thus usually indicate the need for surgery. 2 In the United States in 2009, there were more than 3600 hospital discharges for spinal surgery to correct adolescent idiopathic scoliosis, the total costs of which (approximately $514 million) ranked second only to appendicitis among children 10 to 17 years of age.3
Treatment with rigid bracing (thoracolumbosacral orthosis) is the most common nonoperative treatment for the prevention of curve progression. There are many different brace designs, but with all of them, the objective is to restore the normal contours and alignment of the spine by means of external forces and, in some designs, the stimulation of active correction as the patient moves the spine away from pressures within the brace.
Studies of bracing in adolescent idiopathic scoliosis have suggested that bracing decreases the risk of curve progression.4-10 However, the results were inconsistent, the studies were observational, and only one prospective study enrolled both patients who underwent bracing and those who did not.11,12 Thus, the effect of bracing on curve progression and rate of surgery has remained unclear. We conducted the Bracing in Adolescent Idiopathic Scoliosis Trial (BRAIST) to determine the effectiveness of bracing, as compared with observation, in preventing progression of the curve to 50 degrees or more (a common indication for surgery).
Methods
Study Design
We conducted BRAIST in 25 institutions across the United States and Canada. Enrollment began in March 2007. Initially, the trial was designed solely as a randomized trial. However, enrollment was slower than anticipated, because centers screened fewer eligible patients than anticipated and fewer families accepted randomization than the expected frequency of 25% of those approached. Since the main reason for declining randomization was a stated preference for one treatment over the other, a preference group was added to the trial in November 2009, which allowed patients to participate by choosing their own treatment. Therefore, the final design included both a randomized cohort and a preference cohort, with identical inclusion criteria, protocols, and outcomes assessments (Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Enrollment was completed in February 2011.
The study was approved by the human subjects committee at each institution and was overseen by an independent data and safety monitoring board appointed by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The first and second authors take full responsibility for the completeness and integrity of the data reported and for the adherence of the study to the protocol, available at NEJM.org. Additional information about the study initiation and progress is available elsewhere.13 The statistical analysis plan is available with the protocol.
Patient Population
The target population for this study was patients with high-risk adolescent idiopathic scoliosis who met current indications for brace treatment: an age of 10 to 15 years, skeletal immaturity (defined as a Risser grade [a measure of the amount of ossification and eventual fusion of the iliac apophysis, on a scale of 0 to 5, with higher grades indicating greater skeletal maturity] of 0, 1, or 214), and a Cobb angle for the largest curve of 20 to 40 degrees.15 To be eligible, patients could not have received previous treatment for adolescent idiopathic scoliosis (Table S2 in the Supplementary Appendix). Eligibility was determined by the local investigators. Standard information about the trial was presented to eligible patients by means of an online education module.
Patients who declined participation in the study were registered as screened, and their age, sex, race and ethnic group, curve type,16 Cobb angle of the largest curve, and reason for declining were recorded in a Web-based enrollment system. Patients providing assent to randomization received a computer-generated assignment to bracing or observation, which was stratified according to curve type (single thoracic curve vs. all other curves); patients in the preference cohort chose bracing or observation. Written informed consent from the parent or guardian was required before any study procedures were initiated.
Study Interventions
Patients in the observation group received no specific treatment. Patients in the bracing group received a rigid thoracolumbosacral orthosis, prescribed to be worn for a minimum of 18 hours per day. Participating centers prescribed the type of brace used in their normal clinical practice. Wear time was determined by means of a temperature logger (StowAway or TidbiT data logger, Onset Computer) embedded in the brace and programmed to log the date, time, and temperature every 15 minutes. A temperature of 28.0°C (82.4°F) or higher17,18 indicated that the brace was being worn. Patients who received a brace were considered to be treated, regardless of their level of compliance with prescribed brace wear.
Both patients and clinicians were aware of the assigned treatment. However, all radiographic evaluations and outcome determinations were made at the central coordinating center by two readers (a research associate and a musculoskeletal radiologist) who were unaware of the treatment assignment and the treatment received.
Data-Collection and Follow-up Periods
We collected radiographic, clinical, orthotic, and self-reported data at 6-month intervals. Adverse events and quality-of-life scores were monitored at each follow-up assessment and reported to the data and safety monitoring board. A complete list of these data is provided in Table S3 in the Supplementary Appendix. The type of brace (Boston, Wilmington, or one of several other designs), specific customizations, and modifications over time were recorded. Temperature-monitor data were downloaded every 6 months by the research coordinator.
Outcomes
The primary outcome was determined when the first of two conditions was met: curve progression to 50 degrees or more (treatment failure) or skeletal maturity without this degree of curve progression (treatment success). The original maturity outcome was based on the change in vertical height, with adjustment for the change in the Cobb angle.19 Owing to concerns regarding the accuracy and reliability of this measure, maturity was redefined as a Risser grade of 4 for girls (75 to 100% ossification of the iliac apophysis, corresponding to near-cessation of growth) or 5 for boys (100% ossification of the apophysis with fusion to the ilium) and a Sanders digital maturity stage of 7 (defined as closure of all physes of the phalanges).20 This change was made before any analysis of the data. In the case of disagreement between the two primary readers regarding the treatment outcome, a third reader who was unaware of the treatment assignment and the treatment received broke the tie.
The score on the Pediatric Quality of Life Inventory (PedsQL), a generic quality-of-life instrument used in studies of acute and chronic illness, was a secondary outcome.21,22 PedsQL scores range from 0 to 100, with higher scores indicating a better quality of life. Other secondary outcomes (not reported here) included health and functioning,23 self-image,24 and perception of spinal appearance.25
Statistical Analysis
The initial sample-size calculations assumed randomization and an equal number of patients in each study group. The treatment-failure rate for bracing was set at 15% on the basis of the literature and the consensus of the protocol-development committee. A survey of potential study participants indicated that at least a 50% reduction in the risk of curvature progression warranting surgery would be required for patients to choose bracing,26 so the treatment-failure rate in the observation group was set at 30%. With an alpha level set at 0.05, a power of 90%, and allowance for a 10% loss to follow-up, we calculated that a sample of 384 patients was required.
The statistical analysis plan prespecified a primary analysis that included data from the combined randomized and preference cohorts according to the treatment received and a secondary intention-to-treat analysis that included data only from the randomized cohort. In both analyses, we used logistic regression to estimate the odds ratio for successful treatment (indicated by skeletal maturity with a Cobb angle of <50 degrees) in the bracing group, as compared with the observation group.
In the primary analysis, we used propensity-score adjustment to control for potential selection bias due to nonrandom treatment assignment in the preference cohort.27 The propensity-score–derivation model was constructed with the use of multivariable logistic regression, with bracing as the dependent variable. We made an a priori decision to include the baseline age and the Cobb angle of the largest curve, along with a variable indicating whether the patient had undergone randomization. Additional variables, with no missing values, that were unbalanced between the study groups at a significance level of 0.05 were also considered for inclusion. The treatment effect was defined as the odds of success as a function of the treatment received, with adjustment for the duration of follow-up and quintiles of the propensity score.
Prespecified interim analyses were performed as requested by the data and safety monitoring board. The cumulative type I error rate was maintained at the planned level of 0.05 by means of the Lan–DeMets28 spending-function approach with the O’Brien–Fleming29 spending function. In addition to the effectiveness analysis, the data and safety monitoring board requested periodic evaluation of the patients’ first 6 months of temperature-monitor data to assess whether patients were complying with the treatment at a level that would allow us to observe a treatment effect if, in fact, one existed. The average time (in hours) of brace wear per day was calculated and divided into quartiles. The chi-square test was used to assess the association between wear time and the rate of success.
Results
Early Termination of the Effectiveness Study
The first interim analysis (September 2012) included 178 patients, and the second (January 2013) included 230 patients. The prespecified P value for stopping the study because of efficacy was 0.00821. The primary analysis yielded an adjusted odds ratio of 2.03 (95% confidence interval [CI], 1.12 to 3.68; P=0.0197), indicating a treatment benefit in favor of bracing. The data and safety monitoring board recommended termination of the trial not only on the basis of this analysis (with the P value close to the prespecified level for study termination) but also on the basis of the results of the intention-to-treat analysis and the observation of a strong positive association between the amount of time spent wearing the brace and the rate of success. The data and safety monitoring board instructed the study team to perform a data lock on all outcomes up to and including the date of the board meeting. The analyses presented in this article were performed with the use of the resulting data set.
Characteristics of the Patients
Of 1183 patients screened, 1086 met the inclusion criteria and made a decision concerning study participation (Figure 1). A total of 383 patients (35%) provided assent, with written informed consent provided by a parent or guardian. These patients then either underwent randomization (155 patients [40%]) or declined randomization and instead chose their treatment (228 [60%]). The 383 patients with informed consent and the 703 who declined participation were similar with respect to age and sex distribution, but in the group with informed consent there was a slightly higher percentage of blacks and a slightly lower percentage of patients with a single lumbar curve or both a thoracic and a thoracolumbar curve (Table S4 in the Supplementary Appendix).
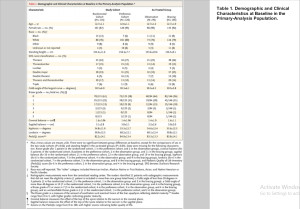
Primary Analysis
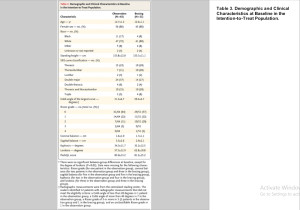
A total of 242 patients were included in the primary analysis: 116 patients (48%) in the randomized cohort and 126 (52%) in the preference cohort (Table 1). The two cohorts differed significantly at baseline with respect to sex distribution, the interval between the diagnosis of scoliosis and trial enrollment, the person who first noticed the scoliosis, and the largest degree of apical vertebral rotation (Table S5 in the Supplementary Appendix).
A total of 146 patients (60%) received a brace, and 96 (40%) underwent observation only. The two study groups were generally similar with respect to baseline characteristics, except that the patients in the bracing group were taller on average than those in the observation group (156.5 cm vs. 153.6 cm, P=0.03). The propensity-score model included baseline height, Cobb angle of the largest curve, age, and status with respect to randomization. The average duration of follow-up was 21.3 months in the observation group and 24.2 months in the bracing group (P=0.01).
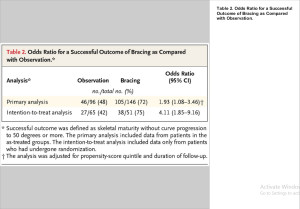
The rate of treatment success was 72% in the bracing group and 48% in the observation group (Table 2). With adjustment for the propensity-score quintile and duration of follow-up, the odds ratio for a successful outcome associated with bracing was 1.93 (95% CI, 1.08 to 3.46). Additional details of the propensity-score modeling are provided in the Supplementary Appendix.
Intention-to-Treat Analysis
A total of 51 patients (44%) in the randomized cohort were assigned to bracing. There were no significant differences at baseline between the bracing and observation groups, except for the degree of lordosis (P=0.02) (Table 3 and Table S6 in the Supplementary Appendix).
The rate of treatment success was 75% among patients randomly assigned to bracing, as compared with 42% among those randomly assigned to observation (unadjusted odds ratio for successful outcome with bracing, 4.11; 95% CI, 1.85 to 9.16) (Table 2). The number needed to treat in order to prevent one case of curve progression warranting surgery was 3.0 (95% CI, 2.0 to 6.2), and the reduction in relative risk with bracing was 56% (95% CI, 26 to 82).
Brace Dose–Response Relationship
The majority of patients assigned to bracing (68%) were treated with a customized Boston-type thoracolumbosacral orthosis. Temperature data were available for 116 patients (from both the randomized and preference cohorts). During the first 6 months, patients wore the brace for a mean (±SD) of 12.1±6.5 hours per day (range, 0 to 23.0). The quartile of duration of brace wear was positively associated with the rate of success (P<0.001). The lowest quartile of wear (mean hours per day, 0 to 6.0) was associated with a success rate (41%) similar to that in the observation group in the primary analysis (48%), whereas brace wear for an average of at least 12.9 hours per day was associated with success rates of 90 to 93%(Figure 2)
Quality of Life and Adverse Events
The average PedsQL scores22 for patients included in the primary and intention-to-treat analyses did not differ significantly between the bracing and observation groups at baseline (Table 1 and Table 3) or at the final follow-up assessment (mean scores in the primary analysis, 82.0 and 81.9, respectively; P=0.97; mean scores in the intention-to-treat analysis, 79.1 and 81.2, respectively; P=0.45) (Tables S7 and S8 in the Supplementary Appendix). There were no significant differences between the bracing and observation groups in the primary analysis with respect to the percentage of patients with any adverse event (P=0.32) or the percentage of patients reporting back pain, the most common adverse event (P=0.29). There was one serious adverse event, a hospitalization for anxiety and depression in a patient who wore a brace. Adverse events involving the skin under the brace were reported in 12 of the 146 patients (8%) who wore a brace.
Figure 1
Study Enrollment and Treatment of the Patients.
Table 1
Demographic and Clinical Characteristics at Baseline in the Primary-Analysis Population.
Table 2
Odds Ratio for a Successful Outcome of Bracing as Compared with Observation.
Table 3
Demographic and Clinical Characteristics at Baseline in the Intention-to-Treat Population.
Figure 2
Rate of Treatment Success According to Average Hours of Daily Brace Wear.
Discussion
In adolescents with idiopathic scoliosis who were considered to be at high risk for curve progression that would eventually warrant surgery, bracing was associated with a significantly greater likelihood of reaching skeletal maturity with a curve of less than 50 degrees, as compared with observation alone. A significant benefit of bracing was observed in both the randomized and the as-treated populations. We also found a significant association between the average hours of daily brace wear and the likelihood of a successful outcome. These findings corroborate those of previous prospective observational studies, which have shown a significantly lower rate of surgery among patients who wore a brace than among those who were untreated12 and a strong brace dose–response relationship.30
The rates of treatment failure in both groups in the randomized cohort were higher than expected, at 25% with bracing and 58% with observation; we hypothesized that the rates would be 15% and 30%, respectively. In previous studies, the rates of progression warranting surgery have varied widely, ranging from 0 to 79% after bracing4,12,31 and from 10 to 38% in untreated patients.12,32-34 This variation could be due to differences in case mix, inconsistent indications for surgery, differences in the quality of the brace and in patient compliance with brace wear, and nonblinded outcome evaluation.
Strengths of this study include the objective monitoring of the time spent wearing the brace; blinded, independent determination of the outcome; the diversity of participating sites; and the a priori determination of the magnitude of risk reduction that was considered necessary by patients in order for them to choose bracing. The independent, blinded documentation of the outcome of a large group of untreated patients can serve as a benchmark in future studies of treatment for this condition.
BRAIST began as a randomized trial, but we were aware at the inception of the study that the majority of families would decline participation in order to pursue their own treatment preferences.26 Therefore, the relatively low enrollment rate and the need to include the preference cohort were not unexpected but resulted in a primary analysis that was an as-treated assessment rather than an intention-to-treat assessment. Potential bias due to nonrandom treatment assignment in this analysis is expected to be minimized, but is not eliminated, by the use of propensity-score adjustment. In addition, the brace dose–response analysis may be confounded by factors such as curve type, curve flexibility, and characteristics of the brace. The observation that the intention-to-treat analysis yielded results that were similar to those of the as-treated analysis provides strong support for the conclusion that bracing reduces the risk of curve progression and the need for surgery.
Our findings have direct clinical applicability because they are derived from assessment of a group of patients for whom bracing would have been recommended in a typical orthopedic practice but in the absence of rigorous supporting data. It is also relevant that, in the primary analysis, 48% of the patients in the observation group had a successful outcome, as did 41% of the patients in the bracing group who spent little time actually wearing the brace. As others have suggested,12,35 current bracing indications may be too broad, resulting in unnecessary treatment for many patients. It is important to identify patients at high risk for clinically significant curve progression who are also most likely to benefit from bracing.
In conclusion, bracing significantly decreased the progression of high-risk curves to the threshold for surgery in patients with adolescent idiopathic scoliosis. Longer hours of brace wear were associated with greater benefit.
The views expressed in this article are those of the authors and do not necessarily represent the official views of any of the funding institutions.
Supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R21AR049587 and R01AR052113, to Dr. Weinstein), the Children’s Miracle Network (to Dr. Weinstein), the Canadian Institutes of Health Research (FRN-81050, to Dr. Wright), the Shriners Hospitals for Children (79125, to Dr. Dobbs), the University of Rochester, and the Children’s Mercy Hospitals and Clinics.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
No potential conflict of interest relevant to this article was reported.
This article was published on September 19, 2013, at NEJM.org.
We thank the many patients and families who participated in this trial and the research coordinators and staff at the participating institutions.
SOURCE INFORMATION
From the Department of Orthopedics and Rehabilitation, University of Iowa, Iowa City (S.L.W., L.A.D.); the Department of Orthopedic Surgery, Hospital for Sick Children, Toronto (J.G.W.); and the Department of Orthopedic Surgery, Washington University School of Medicine and St. Louis Shriners Hospital for Children, St. Louis (M.B.D.).
Address reprint requests to Dr. Weinstein at the Department of Orthopedics and Rehabilitation, University of Iowa, 200 Hawkins Dr., Iowa City, IA 52242, or at stuart-weinstein@uiowa.edu.
References
1. Nachemson AL, Lonstein JE, Weinstein SL. Report of the Prevalence and Natural History Committee of the Scoliosis Research Society. Denver: Scoliosis Research Society, 1982.
2. Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447-455
Web of Science | Medline
3. HCUP Kids’ Inpatient Database (KID). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality, 2009 (http://www.hcup-us.ahrq.gov/kidoverview.jsp).
4. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976;32:Suppl:S91-S100
CrossRef | Web of Science
5. Dolan LA, Weinstein SL. Best treatment for adolescent idiopathic scoliosis: what do current reviews tell us? In: Wright JG, ed. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders, 2009.
6. Focarile FA, Bonaldi A, Giarolo MA, Ferrari U, Zilioli E, Ottaviani C. Effectiveness of nonsurgical treatment for idiopathic scoliosis: overview of available evidence. Spine (Phila Pa 1976;16:395-401
CrossRef | Web of Science
7. Lenssinck ML, Frijlink AC, Berger MY, Bierman-Zeinstra SM, Verkerk K, Verhagen AP. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther 2005;85:1329-1339
Web of Science | Medline
8. Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev 2010;1:CD006850-CD006850
Web of Science | Medline
9. Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am 1997;79:664-674
Web of Science | Medline
10. Screening for idiopathic scoliosis in adolescents. Rockville, MD: Preventive Services Task Force, June 2004 (http://www.uspreventiveservicestaskforce.org/uspstf/uspsaisc.htm).
11. Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:815-822
Web of Science | Medline
12. Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine (Phila Pa 1976;32:2198-2207
CrossRef
13. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine 2013 September 10 (Epub ahead of print).
14. Risser JC. The classic: the iliac apophysis: an invaluable sign in the management of scoliosis — 1958. Clin Orthop Relat Res 2010;468:643-653
CrossRef | Web of Science | Medline
15. Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976;30:2068-2075
CrossRef | Web of Science
16. The Terminology Committee of the Scoliosis Research Society. A glossary of scoliosis terms. Spine 1976;1:57-58 CrossRef
17. Dolan LA, Weinstein SL, Adams BS. Temperature as a diagnostic test for compliance with a thoracolumbosacral orthosis. Presented at the Annual Meeting of the Pediatric Orthopaedic Society of North America, Waikaloa, HI, May 3–7, 2010 (poster).
18. Helfenstein A, Lankes M, Ohlert K, et al. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine (Phila Pa 1976;31:339-344
CrossRef | Web of Science
19. Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B 2005;14:320-324
CrossRef | Web of Science | Medline
20. Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 2008;90:540-553
CrossRef | Web of Science | Medline
21. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329-341
CrossRef | Web of Science | Medline
22. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800-812
CrossRef | Web of Science | < a href=”http://www.ncbi.nlm.nih.gov/pubmed/11468499?dopt=Abstract” target=”_blank”>Medline
23. Landgraf J, Abetz L, Ware J. The CHQ user’s manual. Boston: The Health Institute, New England Medical Center, 1996.
24. Petersen A, Schulenberg J, Abramowitz R, Offer D, Jarcho H. A self-image questionnaire for young adolescents (SIQYA): reliability and validity. J Youth Adolesc 1984;13:93-111
CrossRef | Web of Science | Medline
25. Sanders JO, Harrast JJ, Kuklo TR, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine (Phila Pa 1976;32:2719-2722
CrossRef
26. Dolan LA, Sabesan V, Weinstein SL, Spratt KF. Preference assessment of recruitment into a randomized trial for adolescent idiopathic scoliosis. J Bone Joint Surg Am 2008;90:2594-2605
CrossRef | Web of Science | Medline
27. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41-55
CrossRef | Web of Science
28. Lan KKG, DeMets DL. Changing frequency of interim analysis in sequential monitoring. Biometrics 1989;45:1017-1020
CrossRef | Web of Science | Medline
29. O’Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics 1979;35:549-556
CrossRef | Web of Science | Medline
30. Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010;92:1343-1352
CrossRef | Web of Science | Medline
31. Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH. A comparison of the thoracolumbosacral orthoses and Providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop 2007;27:369-374
CrossRef | Medline
32. Fernandez-Feliberti R, Flynn J, Ramirez N, Trautmann M, Alegria M. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop 1995;15:176-181
Web of Science | Medline
33. Goldberg CJ, Dowling FE, Hall JE, Emans JB. A statistical comparison between natural history of idiopathic scoliosis and brace treatment in skeletally immature adolescent girls. Spine (Phila Pa 1976;18:902-908
CrossRef | Web of Science
34. Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine (Phila Pa 1976;26:42-47
CrossRef | Web of Science
35. Sanders JO, Newton PO, Browne RH, Herring AJ. Bracing in adolescent idiopathic scoliosis, surrogate outcomes, and the number needed to treat. J Pediatr Orthop 2012;32:Suppl 2:S153-S157
CrossRef | Medline
Citing Articles
1. Stavros Pellios, Eustathios Kenanidis, Michael Potoupnis, Eleftherios Tsiridis, Fares E. Sayegh, John Kirkos, George A. Kapetanos. (2016) Curve progression 25 years after bracing for adolescent idiopathic scoliosis: long term comparative results between two matched groups of 18 versus 23 hours daily bracing. Scoliosis and Spinal Disorders 11
CrossRef
2. Kishore Mulpuri, Emily K. Schaeffer, Simon P. Kelley, Pablo Castañeda, Nicholas M. P. Clarke, Jose A. Herrera-Soto, Vidyadhar Upasani, Unni G. Narayanan, Charles T. Price. (2016) What Is the Impact of Center Variability in a Multicenter International Prospective Observational Study on Developmental Dysplasia of the Hip?. Clinical Orthopaedics and Related Research® 474, 1138-1145
CrossRef
3. John P. Dormans. (2016) 2015 SRS Presidential Address: The Next 50 Years. Spine Deformity 4, 167-172
CrossRef
4. Benlong Shi, Jing Guo, Saihu Mao, Zhiwei Wang, Fiona W.P. Yu, Kwong Man Lee, Bobby K.W. Ng, Zezhang Zhu, Yong Qiu, Jack C.Y. Cheng, Tsz Ping Lam. (2016) Curve Progression in Adolescent Idiopathic Scoliosis With a Minimum of 2 Years’ Follow-up After Completed Brace Weaning With Reference to the SRS Standardized Criteria. Spine Deformity 4, 200-205
CrossRef
5. Hans-Rudolf Weiss, Deborah Turnbull, Nicos Tournavitis, Maksym Borysov. (2016) Treatment of Scoliosis-Evidence and Management (Review of the Literature). Middle East Journal of Rehabilitation and Health In Press
CrossRef
6. Claudio Vergari, Isabelle Courtois, Eric Ebermeyer, Houssam Bouloussa, Raphaël Vialle, Wafa Skalli. (2016) Experimental validation of a patient-specific model of orthotic action in adolescent idiopathic scoliosis. European Spine Journal
CrossRef
7. Xin-Kui Li, Zhi-Gang Wu, Hai-Qiang Wang. (2016) Adolescent Idiopathic Scoliosis in China. SPINE 41, 369-370
CrossRef
8. Tamir Ailon, Durga R. Sure, Justin S. Smith, Christopher I. Shaffrey. (2016) Surgical considerations for major deformity correction spine surgery. Best Practice & Research Clinical Anaesthesiology 30, 3-11
CrossRef
9. Søren Ohrt-Nissen, Dennis W. Hallager, Jeppe L. Henriksen, Martin Gehrchen, Benny Dahl. (2016) Curve Magnitude in Patients Referred for Evaluation of Adolescent Idiopathic Scoliosis: Five Years’ Experience From a System Without School Screening. Spine Deformity 4, 120-124
CrossRef
10. N. Cobetto, C. E. Aubin, S. Parent, J. Clin, S. Barchi, I. Turgeon, Hubert Labelle. (2016) Effectiveness of braces designed using computer-aided design and manufacturing (CAD/CAM) and finite element simulation compared to CAD/CAM only for the conservative treatment of adolescent idiopathic scoliosis: a prospective randomized controlled trial. European Spine Journal
CrossRef
11. Edmond H. M. Lou, Douglas L. Hill, Jim V. Raso, Marc Moreau, Douglas Hedden. (2016) How quantity and quality of brace wear affect the brace treatment outcomes for AIS. European Spine Journal 25, 495-499
CrossRef
12. Saihu Mao, Benlong Shi, Leilei Xu, Zhiwei Wang, Alec Lik Hang Hung, Tsz Ping Lam, Fiona Wai Ping Yu, Kwong Man Lee, Bobby Kin Wah Ng, Jack Chun Yiu Cheng, Zezhang Zhu, Yong Qiu. (2016) Initial Cobb angle reduction velocity following bracing as a new predictor for curve progression in adolescent idiopathic scoliosis. European Spine Journal 25, 500-505
CrossRef
13. R.M. Houwert, M.H.J. Verhofstad, F. Hietbrink, M.C. Kruyt. (2016) De conventionele RCT voor trauma- en orthopedisch chirurgen: geen heilige graal. Nederlands Tijdschrift voor Traumachirurgie 24, 2-5
CrossRef
14. Traci Schwieger, Shelly Campo, Stuart L. Weinstein, Lori A. Dolan, Sato Ashida, Keli R. Steuber. (2016) Body Image and Quality-of-Life in Untreated Versus Brace-Treated Females With Adolescent Idiopathic Scoliosis. SPINE 41, 311-319
CrossRef
15. Wei-Pin Chang, Yaleng Lin, Hsiao-Ling Huang, Hsing-Fang Lu, Shih-Tien Wang, Ying-Chen Chi, Kuo-Sheng Hung, Hsiang-Yin Chen. (2016) Scoliosis and the Subsequent Risk of Depression. SPINE 41, 253-258
CrossRef
16. Elias Dakwar, Armen Deukmedjian, Yoav Ritter, C. Dain Allred, Glenn R. Rechtine. . Spinal Pathology, Conditions, and Deformities. 2016:, 584-611.
CrossRef
17. C. Rami-Colás, A.M. Martín-Nogueras. (2016) Tratamiento de fisioterapia de la escoliosis idiopática: Schroth versus gimnasia Abdominal Hipopresiva. Fisioterapia 38, 28-37
CrossRef
18. Gabriel Gutman, Mathieu Benoit, Julie Joncas, Marie Beauséjour, Soraya Barchi, Hubert Labelle, Stefan Parent, Jean-Marc Mac-Thiong. (2016) The effectiveness of the SpineCor brace for the conservative treatment of adolescent idiopathic scoliosis. Comparison with the Boston brace. The Spine Journal
CrossRef
19. Cindy L. Marti, Steven D. Glassman, Patrick T. Knott, Leah Y. Carreon, Michael T. Hresko. (2015) Scoliosis Research Society members attitudes towards physical therapy and physiotherapeutic scoliosis specific exercises for adolescent idiopathic scoliosis. Scoliosis 10
CrossRef
20. Sanja Schreiber, Eric C. Parent, Elham Khodayari Moez, Douglas M. Hedden, Doug Hill, Marc J. Moreau, Edmond Lou, Elise M. Watkins, Sarah C. Southon. (2015) The effect of Schroth exercises added to the standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis—an assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner”. Scoliosis 10
CrossRef
21. Angelo G. Aulisa, Vincenzo Guzzanti, Francesco Falciglia, Marco Giordano, Emanuele Marzetti, Lorenzo Aulisa. (2015) Lyon bracing in adolescent females with thoracic idiopathic scoliosis: a prospective study based on SRS and SOSORT criteria. BMC Musculoskeletal Disorders 16
CrossRef
22. Hiroshi Kuroki, Naoki Inomata, Hideaki Hamanaka, Kiyoshi Higa, Etsuo Chosa, Naoya Tajima. (2015) Efficacy of the Osaka Medical College (OMC) brace in the treatment of adolescent idiopathic scoliosis following Scoliosis Research Society brace studies criteria. Scoliosis 10
CrossRef
23. Jean Claude de Mauroy, Alexandre Journe, Fabio Gagaliano, Cyril Lecante, Frederic Barral, Sophie Pourret. (2015) The new Lyon ARTbrace versus the historical Lyon brace: a prospective case series of 148 consecutive scoliosis with short time results after 1 year compared with a historical retrospective case series of 100 consecutive scoliosis; SOSORT award 2015 winner. Scoliosis 10
CrossRef
24. Fabio Zaina, Michele Romano, Patrick Knott, Jean Claude de Mauroy, Theodoros B. Grivas, Tomasz Kotwicki, Toru Maruyama, Joseph O’Brien, Manuel Rigo, Stefano Negrini. (2015) Research quality in scoliosis conservative treatment: state of the art. Scoliosis 10
CrossRef
25. Fabio Zaina, Jean Claude de Mauroy, Sabrina Donzelli, Stefano Negrini. (2015) SOSORT Award Winner 2015: a multicentre study comparing the SPoRT and ART braces effectiveness according to the SOSORT-SRS recommendations. Scoliosis 10
CrossRef
26. Hiroshi Kuroki, Naoki Inomata, Hideaki Hamanaka, Kiyoshi Higa, Etsuo Chosa, Naoya Tajima. (2015) Predictive factors of Osaka Medical College (OMC) brace treatment in patients with adolescent idiopathic scoliosis. Scoliosis 10
CrossRef
27. Harald Steen, Johan Emil Lange, Jens Ivar Brox. (2015) Early weaning in idiopathic scoliosis. Scoliosis 10
CrossRef
28. David B. Bumpass, Sara K. Fuhrhop, Mario Schootman, June C. Smith, Scott J. Luhmann. (2015) Vertebral Body Stapling for Moderate Juvenile and Early Adolescent Idiopathic Scoliosis. SPINE 40, E1305-E1314
CrossRef
29. Jason Pui Yin Cheung, Dino Samartzis, Prudence Wing Hang Cheung, Ka Hei Leung, Kenneth Man Chee Cheung, Keith Dip-Kei Luk. (2015) The distal radius and ulna classification in assessing skeletal maturity. Journal of Pediatric Orthopaedics B 24, 546-551
CrossRef
30. J. Matussek, E. Dingeldey, A. Benditz, G. Rezai, K. Nahr. (2015) Konservative Behandlung der idiopathischen Skoliose. Der Orthopäde 44, 869-878
CrossRef J. Matussek, E. Dingeldey, A. Benditz, G. Rezai, K. Nahr. (2015) Konservative Behandlung der idiopathischen Skoliose. Der Orthopäde 44, 869-878
CrossRef
31. C. Vergari, I. Courtois, E. Ebermeyer, H. Bouloussa, R. Vialle, W. Skalli. (2015) Simulation of orthotic treatment in adolescent idiopathic scoliosis using a subject-specific finite element model. Computer Methods in Biomechanics and Biomedical Engineering 18, 2076-2077
CrossRef
32. Wei Hui, Xu Jinyuan, Jiang Zhong, Ye Shuliang, Song Hongquan, Ning Xitao, Huang Huanmin, Chen Wei, Pei Jianwei, Jiang Nengyi, Chen Shao, Du Honggen. (2015) Effect of a Traditional Chinese Medicine combined therapy on adolescent idiopathic scoliosis: a randomized controlled trial. Journal of Traditional Chinese Medicine 35, 514-519
CrossRef
33. Tariq Rahman, Whitney Sample, Petya Yorgova, Geraldine Neiss, Kenneth Rogers, Suken Shah, Peter Gabos, Dan Kritzer, J. Richard Bowen. (2015) Electronic monitoring of orthopedic brace compliance. Journal of Children’s Orthopaedics 9, 365-369
CrossRef
.34 Jack C. Cheng, René M. Castelein, Winnie C. Chu, Aina J. Danielsson, Matthew B. Dobbs, Theodoros B. Grivas, Christina A. Gurnett, Keith D. Luk, Alain Moreau, Peter O. Newton, Ian A. Stokes, Stuart L. Weinstein, R. Geoffrey Burwell. (2015) Adolescent idiopathic scoliosis. Nature Reviews Disease Primers, 15030
CrossRef
35. J.A. Deurloo, P.H. Verkerk. (2015) To screen or not to screen for adolescent idiopathic scoliosis? A review of the literature. Public Health 129, 1267-1272
CrossRef
36. Ane Simony, Steen Bach Christensen, Leah Y. Carreon, Mikkel Osterheden Andersen. (2015) Radiological Outcomes in Adolescent Idiopathic Scoliosis Patients More Than 22 Years After Treatment. Spine Deformity 3, 436-439
CrossRef
37. Robert J. Thorsness, John R. Faust, Caleb J. Behrend, James O. Sanders. (2015) Nonsurgical Management of Early-onset Scoliosis. Journal of the American Academy of Orthopaedic Surgeons 23, 519-528
CrossRef
38. Ximing Xu, Fei Wang, Mingyuan Yang, Qikai Huang, Yifan Chang, Xianzhao Wei, Yushu Bai, Ming Li. (2015) Chinese Adaptation of the Bad Sobernheim Stress Questionnaire for Patients With Adolescent Idiopathic Scoliosis Under Brace Treatment. Medicine 94, e1236
CrossRef
39. Haribalakrishna Balasubramanian, Anitha Ananthan, Shripada Rao, Sanjay Patole. (2015) Odds ratio vs risk ratio in randomized controlled trials. Postgraduate Medicine 127, 359-367
CrossRef
40. Mark A Williams, Peter J Heine, Esther M Williamson, Francine Toye, Melina Dritsaki, Stavros Petrou, Richard Crossman, Ranjit Lall, Karen L Barker, Jeremy Fairbank, Ian Harding, Adrian Gardner, Anne-Marie Slowther, Neil Coulson, Sarah E Lamb, . (2015) Active Treatment for Idiopathic Adolescent Scoliosis (ACTIvATeS): a feasibility study. Health Technology Assessment 19, 1-242
CrossRef
41. D. Y. T. Fong, K. M. C. Cheung, Y. W. Wong, W. Y. Cheung, I. C. Y. Fu, E. E. Kuong, K. C. Mak, M. To, D. Samartzis, K. D. K. Luk. (2015) An alternative to a randomised control design for assessing the efficacy and effectiveness of bracing in adolescent idiopathic scoliosis. The Bone & Joint Journal 97-B, 973-981
CrossRef
42. Amer F. Samdani, Robert J. Ames, Jeff S. Kimball, Joshua M. Pahys, Harsh Grewal, Glenn J. Pelletier, Randal R. Betz. (2015) Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. European Spine Journal 24, 1533-1539
CrossRef
43. Prakash Sitoula, Kushagra Verma, Laurens Holmes, Peter G. Gabos, James O. Sanders, Petya Yorgova, Geraldine Neiss, Kenneth Rogers, Suken A. Shah. (2015) Prediction of Curve Progression in Idiopathic Scoliosis. Spine 40, 1006-1013
CrossRef
44. Stefano Negrini, Silvia Minozzi, Josette Bettany-Saltikov, Nachiappan Chockalingam, Theodoros B. Grivas, Tomasz Kotwicki, Toru Maruyama, Michele Romano, Fabio Zaina, Stefano Negrini. . Braces for idiopathic scoliosis in adolescents. 2015.
CrossRef
45. Min Deng, Steve C.N. Hui, Fiona W.P. Yu, Tsz-Ping Lam, Yong Qiu, Bobby K.W. Ng, Jack C.Y. Cheng, Winnie C.W. Chu. (2015) MRI-based morphological evidence of spinal cord tethering predicts curve progression in adolescent idiopathic scoliosis. The Spine Journal 15, 1391-1401
CrossRef
46. Bareket Falk, W. Alan Rigby, Nasreen Akseer. (2015) Adolescent idiopathic scoliosis: the possible harm of bracing and the likely benefit of exercise. The Spine Journal 15, 1169-1171
CrossRef
47. Marie Beauséjour, Lise Goulet, Debbie Ehrmann Feldman, Roxane Borgès Da Silva, Raynald Pineault, Michel Rossignol, Marjolaine Roy-Beaudry, Hubert Labelle. (2015) Pathways of healthcare utilisation in patients with suspected adolescent idiopathic scoliosis: a cross-sectional study. BMC Health Services Research 15
CrossRef
48. Kai Li, Sheng Zhao, Xiaochun Wei, Xiaoqiang Wang, Jian Sun, Yao He, Junping Zhen. (2015) A Preliminary Study on a Novel Growth Guidance Rod System for Early-Onset Scoliosis in a Sheep Model. Spine 40, 767-772
CrossRef
49. Daniel Y.T. Fong, Kenneth M.C. Cheung, Yat-Wa Wong, Yuen-Yin Wan, Chun-Fan Lee, Tsz-Ping Lam, Jack C.Y. Cheng, Bobby K.W. Ng, Keith D.K. Luk. (2015) A population-based cohort study of 394,401 children followed for 10 years exhibits sustained effectiveness of scoliosis screening. The Spine Journal 15, 825-833
CrossRef
50. Joon-Hyuk Park, Paul Stegall, Sunil K. Agrawal. . (2015) Dynamic brace for correction of abnormal postures of the human spine. , 5922-5927
CrossRef
51. Francesc Malagelada, Mathew D. Sewell, Amr Fahmy, Alexander Gibson. (2015) Long-term clinical and radiological outcomes of Copenhagen syndrome with 19 affected levels: a case report. The Spine Journal 15, e19-e23
CrossRef
52. Suken A. Shah. (2015) Nonoperative treatment for adolescent idiopathic scoliosis. Seminars in Spine Surgery 27, 27-32
CrossRef
53. A. Noelle Larson, Baron S. Lonner. (2015) Comparative effectiveness of implant density. Seminars in Spine Surgery 27, 45-51
CrossRef
54. Eric Chalmers, Witold Pedrycz, Edmond Lou. (2015) Human Experts’ and a Fuzzy Model’s Predictions of Outcomes of Scoliosis Treatment: A Comparative Analysis. IEEE Transactions on Biomedical Engineering 62, 1001-1007
CrossRef
55. Amer F. Samdani, Randal R. Betz. (2015) Growth modulation techniques for adolescent idiopathic scoliosis. Seminars in Spine Surgery 27, 52-57
CrossRef
56. Eric Chalmers, Edmond Lou, Doug Hill, H. Vicky Zhao. (2015) An advanced compliance monitor for patients undergoing brace treatment for idiopathic scoliosis. Medical Engineering & Physics 37, 203-209
CrossRef
56. Claudio Vergari, Gwenael Ribes, Benjamin Aubert, Clayton Adam, Lotfi Miladi, Brice Ilharreborde, Kariman Abelin-Genevois, Philippe Rouch, Wafa Skalli. (2015) Evaluation of a Patient-Specific Finite-Element Model to Simulate Conservative Treatment in Adolescent Idiopathic Scoliosis. Spine Deformity 3, 4-11
CrossRef
58. Fabio Zaina, Michele Romano, Sabrina Donzelli, Stefano Negrini. (2015) Letter to the Editor concerning the Article “Adolescent Idiopathic Scoliosis: A 71 Cases Study Ascertaining That Straightening Is Possible, and a New Etiological Hypothesis”. Asian Spine Journal 9, 306
CrossRef
59. Christian Wong. (2015) Mechanism of right thoracic adolescent idiopathic scoliosis at risk for progression; a unifying pathway of development by normal growth and imbalance. Scoliosis 10, 2
CrossRef
60. Nasreen Akseer, Kimberly Kish, W Rigby, Matthew Greenway, Panagiota Klentrou, Philip M Wilson, Bareket Falk. (2015) Does bracing affect bone health in women with adolescent idiopathic scoliosis?. Scoliosis 10, 5
CrossRef
61. Toru Maruyama, Yosuke Kobayashi, Makoto Miura, Yusuke Nakao. (2015) Effectiveness of brace treatment for adolescent idiopathic scoliosis. Scoliosis 10, S12
CrossRef
62. Minnella Salvatore, Zaina Fabio, Romano Michele, Negrini Alessandra, Negrini Stefano, Loren M. Fishman, Erik J. Groessl, Karen J. Sherman. (2015) Serial Case Reporting Yoga for Idiopathic and Degenerative Scoliosis. Global Advances in Health and Medicine 4, 79-80
CrossRef
63. Yizhar Floman, Gheorghe Burnei, Stefan Gavriliu, Yoram Anekstein, Sergiu Straticiuc, Miklos Tunyogi-Csapo, Yigal Mirovsky, Daniel Zarzycki, Tomasz Potaczek, Uri Arnin. (2015) Surgical management of moderate adolescent idiopathic scoliosis with ApiFix®: a short peri- apical fixation followed by post-operative curve reduction with exercises. Scoliosis 10, 4
CrossRef
64. T. Samuel Pantoja, L. Marcela Chamorro. (2015) Escoliosis en niños y adolescentes. Revista Médica Clínica Las Condes 26, 99-108
CrossRef
65. Laury Cuddihy, Aina J. Danielsson, Patrick J. Cahill, Amer F. Samdani, Harsh Grewal, John M. Richmond, M. J. Mulcahey, John P. Gaughan, M. Darryl Antonacci, Randal R. Betz. (2015) Vertebral Body Stapling versus Bracing for Patients with High-Risk Moderate Idiopathic Scoliosis. BioMed Research International 2015, 1-7
CrossRef
66. Shahnawaz Anwer, Ahmad Alghadir, Md. Abu Shaphe, Dilshad Anwar. (2015) Effects of Exercise on Spinal Deformities and Quality of Life in Patients with Adolescent Idiopathic Scoliosis. BioMed Research International 2015, 1-15
CrossRef
67. Stefano Negrini, Timothy M Hresko, Joseph P O’Brien, Nigel Price, , . (2015) Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non–operative management committee. Scoliosis 10, 8
CrossRef
68. Mark W. Morningstar, Aatif Siddiqui, Clayton J. Stitzel, Brian Dovorany. (2015) Pain and Radiographic Outcomes in Adult Idiopathic Scoliosis Patients Using a Scoliosis Activity Suit: An 18-Month Case Controlled Chart Review. International Journal of Clinical Medicine 06, 597-604
CrossRef
69. Kevin M. Felton, Scott Savage, Lori Karol. (2015) Patient Adherence to Instructions of Weaning into Scoliosis Orthosis Wear. Journal of Prosthetics and Orthotics 27, 23-26
CrossRef
70. Akin Ugras. (2015) Brace Treatment Is Effective for Scoliosis. Orthopedics 38, 6-7
CrossRef
71. Matthew E. Oetgen. (2015) Universal screening for idiopathic scoliosis. Current Orthopaedic Practice 26, 87-88
CrossRef
72. Gregory J. Redding. (2015) Primary Thoraco-spinal Disorders of Childhood. Paediatric Respiratory Reviews 16, 25-29
CrossRef
73. Nathan Evaniew, Tahira Devji, Brian Drew, Devin Peterson, Michelle Ghert, Mohit Bhandari. (2015) The surgical management of scoliosis: a scoping review of the literature. Scoliosis 10, 1
CrossRef
74. Hans-Rudolf Weiss, Alexander Kleban. (2015) Development of CAD/CAM Based Brace Models for the Treatment of Patients with Scoliosis-Classification Based Approach versus Finite Element Modelling. Asian Spine Journal 9, 661
CrossRef
75. Eric Chalmers, Doug Hill, Vicky Zhao, Edmond Lou. (2015) Prescriptive analytics applied to brace treatment for AIS: a pilot demonstration. Scoliosis 10, S13
CrossRef
76. Amir Khoshbin, Liora Caspi, Peggy W. Law, Sandra Donaldson, Derek Stephens, Trevor da Silva, Catharine S. Bradley, James G. Wright. (2015) Outcomes of Bracing in Juvenile Idiopathic Scoliosis Until Skeletal Maturity or Surgery. Spine 40, 50-55
CrossRef
77. G. De Korvin, T. Randriaminahisoa, E. Cugy, L. Cheze, M. de Sèze. (2014) Detection of progressive idiopathic scoliosis during growth using back surface topography: A prospective study of 100 patients. Annals of Physical and Rehabilitation Medicine 57, 629-639
CrossRef
78. Daniel D. Bohl, Connor J. Telles, Nicholas S. Golinvaux, Bryce A. Basques, Peter A. DeLuca, Jonathan N. Grauer. (2014) Effectiveness of Providence Nighttime Bracing in Patients With Adolescent Idiopathic Scoliosis. Orthopedics 37, e1085-e1090
CrossRef
79. Ron El-Hawary, Chukwudi Chukwunyerenwa. (2014) Update on Evaluation and Treatment of Scoliosis. Pediatric Clinics of North America 61, 1223-1241
CrossRef
80. Raphael D Adobor, Paal Joranger, Harald Steen, Ståle Navrud, Jens Ivar Brox. (2014) A health economic evaluation of screening and treatment in patients with adolescent idiopathic scoliosis. Scoliosis 9
CrossRef
81. J. G. Buchan, D. M. Alvarado, G. E. Haller, C. Cruchaga, M. B. Harms, T. Zhang, M. C. Willing, D. K. Grange, A. C. Braverman, N. H. Miller, J. A. Morcuende, N. L.-S. Tang, T.-P. Lam, B. K.-W. Ng, J. C.-Y. Cheng, M. B. Dobbs, C. A. Gurnett. (2014) Rare variants in FBN1 and FBN2 are associated with severe adolescent idiopathic scoliosis. Human Molecular Genetics 23, 5271-5282
CrossRef
82. Yang-Sun Park, Young-Tae Lim. (2014) Effects of the Functional Garment Wear on Cobb’s Angle and COM of Trunk and Pelvic during Gait for Adolescent Idiopathic Scoliosis Patients. Korean Journal of Sport Biomechanics 24, 269-275
CrossRef
83. Monia Lusini, Sabrina Donzelli, Salvatore Minnella, Fabio Zaina, Stefano Negrini. (2014) Brace treatment is effective in idiopathic scoliosis over 45°: an observational prospective cohort controlled study. The Spine Journal 14, 1951-1956
CrossRef
84. Amer F. Samdani, Robert J. Ames, Jeff S. Kimball, Joshua M. Pahys, Harsh Grewal, Glenn J. Pelletier, Randal R. Betz. (2014) Anterior Vertebral Body Tethering for Idiopathic Scoliosis. Spine 39, 1688-1693
CrossRef
85. Alexander R. Vaccaro, Charles G. Fisher. (2014) Commentary. Spine 39, E1181-E1182
CrossRef
86. Alexander R. Vaccaro, Charles G. Fisher, Peter G. Whang, Alpesh A. Patel, Ken C. Thomas, Kishore Mulpuri, John Chi, Srinivas K. Prasad. (2014) Evidence-Based Recommendations for Spine Surgery. Spine 39, E1183-E1189
CrossRef
87. J. Matussek, E. Dingeldey, F. Wagner, G. Rezai, K. Nahr. (2014) Konservative Therapie der idiopathischen Skoliose mit dem Korsett. Der Orthopäde 43, 689-702
CrossRef
88. Marco Monticone, Emilia Ambrosini, Daniele Cazzaniga, Barbara Rocca, Simona Ferrante. (2014) Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. European Spine Journal 23, 1204-1214
CrossRef
89. (2014) Bracing adolescents with idiopathic scoliosis. Journal of Paediatrics and Child Health 50:10.1111/jpc.2014.50.issue-5, 415-416
CrossRef
90. Ian W. Nelson. (2014) Funnel plots and spine surgery: unit level and surgeon level outcome data. European Spine Journal 23, 4-5
CrossRef
91. (2014) Effects of Bracing in Adolescents with Idiopathic Scoliosis. New England Journal of Medicine 370:7, 680-681
Free Full Text
92. W. Hennrikus. (2014) Effects of Bracing in Adolescents With Idiopathic Scoliosis. AAP Grand Rounds 31, 14-14
CrossRef
93. Angelo G Aulisa, Vincenzo Guzzanti, Emanuele Marzetti, Marco Giordano, Francesco Falciglia, Lorenzo Aulisa. (2014) Brace treatment in juvenile idiopathic scoliosis: a prospective study in accordance with the SRS criteria for bracing studies – SOSORT award 2013 winner. Scoliosis 9, 3
CrossRef
94. Hak-Sun Kim. (2014) Evidence-Based of Nonoperative Treatment in Adolescent Idiopathic Scoliosis. Asian Spine Journal 8, 695
CrossRef
95. LouAnn Rivett, Aimee Stewart, Joanne Potterton. (2014) The effect of compliance to a Rigo System Cheneau brace and a specific exercise programme on idiopathic scoliosis curvature: a comparative study: SOSORT 2014 award winner. Scoliosis 9, 5
CrossRef
96. Jean de Mauroy, Cyril Lecante, Frédéric Barral, Sophie Pourret. (2014) Prospective study and new concepts based on scoliosis detorsion of the first 225 early in-brace radiological results with the new Lyon brace: ARTbrace. Scoliosis 9, 19
CrossRef
97. Mark Driscoll, Chanel Fortier-Tougas, Hubert Labelle, Stefan Parent, Jean-Marc Mac-Thiong. (2014) Evaluation of an apparatus to be combined with a smartphone for the early detection of spinal deformities. Scoliosis 9, 10
CrossRef
98. Siu Chan, Kenneth MC Cheung, Keith DK Luk, Kenneth WH Wong, Man Wong. (2014) A correlation study between in-brace correction, compliance to spinal orthosis and health-related quality of life of patients with Adolescent Idiopathic Scoliosis. Scoliosis 9, 1
CrossRef
99. Monique S. Burton. (2013) Diagnosis and Treatment of Adolescent Idiopathic Scoliosis. Pediatric Annals 42, e233-e237
CrossRef
100. Carragee , Eugene J. , Lehman , Ronald A. Jr. , . (2013) Spinal Bracing in Adolescent Idiopathic Scoliosis. New England Journal of Medicine 369:16, 1558-1560
Full Text
101. Theodoros B Grivas, Michael Timothy Hresko, Hubert Labelle, Nigel Price, Tomasz Kotwicki, Toru Maruyama. (2013) The pendulum swings back to scoliosis screening: screening policies for early detection and treatment of idiopathic scoliosis – current concepts and recommendations. Scoliosis 8, 16
CrossRef
To the Editor:
Weinstein and colleagues (Oct. 17 issue)1 reported a study evaluating the effect of bracing to decrease curve progression in patients with adolescent idiopathic scoliosis. In the primary analysis, the authors combined data from randomized and preference cohorts and performed a propensity-score analysis to evaluate the effect of bracing. The resulting estimated effect in the primary analysis, which included both cohorts (odds ratio for a successful outcome, 1.93), appears quite different, at least numerically, from that in the randomized cohort alone (odds ratio, 4.11). This suggests either that the model used to create the propensity score may not appropriately capture factors affecting the decision to use bracing or not in each of the two cohorts, or that the underlying true effect of bracing might differ between the two cohorts. In our opinion, the two cohorts should be analyzed separately, providing one odds ratio for the randomized cohort (which was reported) and one for the preference cohort (not reported). Then, with the use of meta-analysis, these two estimates might be combined with appropriate caution if there are no concerns about the heterogeneity of the effect between cohorts, or if there are such concerns, potential sources of heterogeneity should be evaluated.
Hajime Uno, Ph.D.
Lee-Jen Wei, Ph.D.
Michael Hughes, Ph.D.
Harvard University, Boston, MA
wei@hsph.harvard.edu
No potential conflict of interest relevant to this letter was reported.
1 Reference
The authors reply: Uno and colleagues suggest that the odds ratio from the primary analysis cohort did not approximate that from the randomized cohort, possibly because selection bias was not removed through propensity-score adjustment, because the treatment effect was not the same in the two cohorts, or both.
As acknowledged in the article, propensity-score adjustment reduces but may not eliminate selection bias. Furthermore, there are other possible reasons for the difference in these estimates. The odds ratio from the randomized cohort is an unadjusted estimate of the effect of receiving a prescription for a brace, whereas the odds ratio from the primary analysis is an adjusted estimate of the effect of actually receiving a brace. Two covariates were included in the primary analysis: the propensity score and the length of follow-up. Length of follow-up (time between consent and study end point) is a function of multiple interacting variables, including baseline factors contributing to the rate of curve progression and maturation (i.e., sex, maturity, Cobb angle, and curve type) and their interaction with treatment factors (including the “dose” of bracing received). Thus, it is perhaps not surprising that the estimates of treatment effect from the primary analysis and the randomized analysis would differ, even if all selection bias had been removed.
In response to their inquiry: we calculated odds ratios associated with receiving a prescription for a brace in both the primary (combined cohort) and preference cohorts, adjusting for propensity scores but not length of follow-up or other covariates. The odds ratio in the combined cohort was 2.45 (95% confidence interval [CI], 1.40 to 4.29), and the odds ratio in the preference cohort was 2.68 (95% CI, 1.01 to 7.11). Thus, although there remains some variation depending on which cohort and which model is used, these findings also affirm the study conclusion that bracing reduces the rates of progression of scoliosis.
Lori A. Dolan, Ph.D.
University of Iowa, Iowa City, IA
James G. Wright, M.D., M.P.H.
Hospital for Sick Children, Toronto, ON, Canada
Stuart L. Weinstein, M.D.
University of Iowa, Iowa City, IA
stuart-weinstein@uiowa.edu
Since publication of their article, the authors report no further potential conflict of interest.